Bloodlet in Out
| Bloodletting | |
|---|---|
 Bloodletting in 1860. | |
| MeSH | D001815 |

Aboriginal Greek painting on a vase, showing a physician (iatros) haemorrhage a patient
Bloodletting (or blood-letting) is the withdrawal of blood from a patient to preclude or cure illness and disease. Bloodletting, whether past a physician or by leeches, was based on an aboriginal system of medicine in which blood and other actual fluids were regarded as "humours" that had to remain in proper residue to maintain health. Information technology is claimed to take been the most common medical practice performed past surgeons from antiquity until the late 19th century, a bridge of over 2,000 years.[i] In Europe, the exercise continued to be relatively common until the end of the 18th century.[2] The practice has now been abandoned past modern-style medicine for all except a few very specific medical conditions.[three] In the overwhelming majority of cases, the historical use of bloodletting was harmful to patients.[four]
Today, the term phlebotomy refers to the drawing of blood for laboratory analysis or blood transfusion.[5] Therapeutic phlebotomy refers to the drawing of a unit of blood in specific cases similar hemochromatosis, polycythemia vera, porphyria cutanea tarda, etc., to reduce the number of blood-red claret cells.[six] [7] The traditional medical exercise of bloodletting is today considered to be a pseudoscience.[8]
In the ancient globe [edit]

A chart showing the parts of the body to be bled for unlike diseases, c. 1310–20

Passages from the Ebers Papyrus may indicate that bloodletting by scarification was an accustomed practise in Aboriginal Egypt.[ix] [10] [11] Egyptian burials accept been reported to contain bloodletting instruments.[12] According to some accounts, the Egyptians based the idea on their observations of the hippopotamus,[13] confusing its red secretions with blood and believing that it scratched itself to relieve distress.[xiv] [15]
In Greece, bloodletting was in use in the fifth century BC during the lifetime of Hippocrates, who mentions this practice but generally relied on dietary techniques.[16] Erasistratus, however, theorized that many diseases were caused by plethoras, or overabundances, in the blood and advised that these plethoras exist treated, initially, by practise, sweating, reduced food intake, and airsickness.[17] His student Herophilus as well opposed bloodletting. But a contemporary Greek doc, Archagathus, one of the first to practice in Rome, did believe in the value of bloodletting.
"Haemorrhage" a patient to health was modeled on the process of period. Hippocrates believed that menstruation functioned to "purge women of bad humours". During the Roman Empire, the Greek physician Galen, who subscribed to the teachings of Hippocrates, advocated physician-initiated bloodletting.[18]
The popularity of bloodletting in the classical Mediterranean world was reinforced by the ideas of Galen, later he discovered that not just veins merely too arteries were filled with blood, not air as was unremarkably believed at the time.[nineteen] [twenty] There were two key concepts in his system of bloodletting. The outset was that blood was created then used up; information technology did not broadcast, and so information technology could "stagnate" in the extremities. The second was that humoral residuum was the ground of illness or health, the iv humours existence blood, phlegm, black bile, and yellow bile, relating to the four Greek classical elements of air, water, globe, and fire respectively. Galen believed that claret was the dominant humor and the one in about need of control. In order to balance the humours, a physician would either remove "backlog" blood (plethora) from the patient or give them an emetic to induce vomiting, or a diuretic to induce urination.
Galen created a complex system of how much claret should exist removed based on the patient's age, constitution, the season, the weather and the identify. "Practice-it-yourself" bleeding instructions following these systems were developed.[21] Symptoms of plethora were believed to include fever, apoplexy, and headache. The claret to be allow was of a specific nature determined by the disease: either arterial or venous, and afar or shut to the expanse of the body affected. He linked different blood vessels with dissimilar organs, co-ordinate to their supposed drainage. For example, the vein in the right manus would be let for liver bug and the vein in the left hand for problems with the spleen. The more severe the affliction, the more blood would exist let. Fevers required copious amounts of bloodletting.
Eye Ages [edit]
The Talmud recommended a specific day of the calendar week and days of the month for bloodletting[ commendation needed ], and similar rules, though less codified, can exist found amidst Christian writings advising which saints' days were favourable for bloodletting.[ citation needed ] During medieval times bleeding charts were common, showing specific bleeding sites on the body in alignment with the planets and zodiacs.[21] Islamic medical authors also advised bloodletting, specially for fevers. Information technology was practised according to seasons and certain phases of the Moon in the lunar calendar. The practice was probably passed by the Greeks with the translation of ancient texts to Standard arabic and is different than bloodletting past cupping mentioned in the traditions of Muhammad. When Muslim theories became known in the Latin-speaking countries of Europe, bloodletting became more than widespread. Together with cautery, it was primal to Arabic surgery; the key texts Kitab al-Qanun and specially Al-Tasrif li-man 'ajaza 'an al-ta'lif both recommended it. It was also known in Ayurvedic medicine, described in the Susruta Samhita.
Use through the 19th century [edit]

Ioannis Sculteti, Armamentium Chirugiae, 1693 – diagrammed transfusion of sheep's blood

Fifty-fifty after the humoral system fell into disuse, the practice was continued by surgeons and hairdresser-surgeons. Though the bloodletting was often recommended past physicians, it was carried out past barbers. This led to the stardom between physicians and surgeons. The ruddy-and-white-striped pole of the barbershop, still in employ today, is derived from this practice: the red symbolizes blood while the white symbolizes the bandages. Bloodletting was used to "treat" a broad range of diseases, becoming a standard treatment for most every disquiet, and was practiced prophylactically likewise as therapeutically.

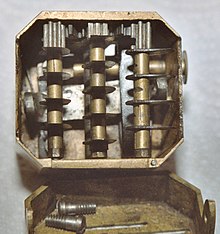

Scarificator, showing depth adjustment bar

Diagram of scarificator, showing depth aligning
A number of dissimilar methods were employed. The most common was phlebotomy, or venesection (often called "breathing a vein"), in which blood was drawn from one or more of the larger external veins, such as those in the forearm or neck. In arteriotomy, an artery was punctured, although generally just in the temples. In scarification (non to be confused with scarification, a method of body modification), the "superficial" vessels were attacked, ofttimes using a syringe, a spring-loaded lancet, or a glass loving cup that independent heated air, producing a vacuum within (see fire cupping). There was as well a specific bloodletting tool called a scarificator, used primarily in 19th century medicine. It has a spring-loaded mechanism with gears that snaps the blades out through slits in the front cover and back in, in a circular move. The example is cast brass, and the mechanism and blades steel. One knife bar gear has slipped teeth, turning the blades in a different direction than those on the other bars. The concluding photograph and the diagram show the depth aligning bar at the back and sides.
Leeches could too be used. The withdrawal of so much blood as to induce syncope (fainting) was considered benign, and many sessions would only stop when the patient began to swoon.
William Harvey disproved the basis of the practice in 1628,[2] and the introduction of scientific medicine, la méthode numérique, allowed Pierre Charles Alexandre Louis to demonstrate that phlebotomy was entirely ineffective in the handling of pneumonia and various fevers in the 1830s. Nevertheless, in 1838, a lecturer at the Royal Higher of Physicians would nevertheless state that "blood-letting is a remedy which, when judiciously employed, it is hardly possible to estimate too highly",[22] and Louis was dogged by the sanguinary Broussais, who could recommend leeches fifty at a time. Some physicians resisted Louis' work because they "were not prepared to discard therapies 'validated by both tradition and their ain experience on account of somebody else'south numbers'."[23]
Bloodletting was used to treat almost every disease. 1 British medical text recommended bloodletting for acne, asthma, cancer, cholera, coma, convulsions, diabetes, epilepsy, gangrene, gout, herpes, indigestion, insanity, jaundice, leprosy, ophthalmia, plague, pneumonia, scurvy, smallpox, stroke, tetanus, tuberculosis, and for some i hundred other diseases. Bloodletting was even used to care for most forms of hemorrhaging such as nosebleed, excessive menstruation, or hemorrhoidal bleeding. Before surgery or at the onset of childbirth, blood was removed to preclude inflammation. Before amputation, it was customary to remove a quantity of blood equal to the amount believed to circulate in the limb that was to be removed.[24]
There were as well theories that bloodletting would cure "heartsickness" and "heartbreak". A French physician, Jacques Ferrand wrote a book in 1623 on the uses of bloodletting to cure a broken heart. He recommended bloodletting to the point of center failure (literal).[25]
Leeches became particularly popular in the early on nineteenth century. In the 1830s, the French imported about forty meg leeches a year for medical purposes, and in the next decade, England imported vi million leeches a year from France alone. Through the early decades of the century, hundreds of millions of leeches were used past physicians throughout Europe.[26]
Bloodletting was also popular in the young United States of America, where Benjamin Rush (a signatory of the Proclamation of Independence) saw the state of the arteries as the central to disease, recommending levels of bloodletting that were high even for the time. George Washington asked to be bled heavily later on he developed a throat infection from weather exposure. Within a x-60 minutes period, a total of 124–126 ounces (3.75 liters) of blood was withdrawn prior to his death from a pharynx infection in 1799.[28]

Bloodsticks for use when bleeding animals
One reason for the continued popularity of bloodletting (and purging) was that, while anatomical knowledge, surgical and diagnostic skills increased tremendously in Europe from the 17th century, the key to curing disease remained elusive, and the underlying belief was that it was better to give any treatment than nothing at all. The psychological benefit of bloodletting to the patient (a placebo effect) may sometimes have outweighed the physiological problems it acquired. Bloodletting slowly lost favour during the 19th century, after French physician Dr. Pierre Louis conducted an experiment in which he studied the effect of bloodletting on pneumonia patients.[29] A number of other ineffective or harmful treatments were available every bit placebos—mesmerism, various processes involving the new technology of electricity, many potions, tonics, and elixirs. Notwithstanding, bloodletting persisted during the 19th century partly because it was readily available to people of any socioeconomic condition.[30]
Controversy and utilize into the 20th century [edit]
Bloodletting gradually declined in popularity over the form of the 19th century, condign rather uncommon in almost places, earlier its validity was thoroughly debated. In the medical customs of Edinburgh, bloodletting was abandoned in practice before it was challenged in theory, a contradiction highlighted past dr.-physiologist John Hughes Bennett.[31] Authorities such equally Austin Flint I, Hiram Corson, and William Osler became prominent supporters of bloodletting in the 1880s and onwards, disputing Bennett's premise that bloodletting had fallen into disuse because it did not work. These advocates framed bloodletting as an orthodox medical exercise, to be used in spite of its full general unpopularity.[32] Some physicians considered bloodletting useful for a more express range of purposes, such every bit to "clear out" infected or weakened blood or its ability to "cause hæmorrhages to cease"—as evidenced in a telephone call for a "off-white trial for claret-letting as a remedy" in 1871.[33]
Some researchers used statistical methods for evaluating handling effectiveness to discourage bloodletting.[29] But at the same time, publications past Philip Pye-Smith and others dedicated bloodletting on scientific grounds.[32]
Bloodletting persisted into the 20th century and was recommended in the 1923 edition of the textbook The Principles and Do of Medicine.[34] The textbook was originally written by Sir William Osler and connected to exist published in new editions under new authors following Osler's death in 1919.[35]
Phlebotomy [edit]
Bloodletting is used today in the handling of a few diseases, including hemochromatosis and polycythemia;[36] however, these rare diseases were unknown and undiagnosable before the advent of scientific medicine. It is skilful past specifically trained practitioners in hospitals, using modern techniques, and is also known equally a therapeutic phlebotomy. In most cases, phlebotomy now refers to the removal of minor quantities of blood for diagnostic purposes. However, in the case of hemochromatosis, bloodletting (by venipuncture) has go the mainstay handling option.[37] [38] In the U.S., according to an bookish article posted in the Journal of Infusion Nursing with information published in 2010, the primary apply of phlebotomy was to take blood that would one day be reinfused back into a person.[39]
In alternative medicine [edit]
Though bloodletting every bit a general health measure has been shown to exist pseudoscience, it is yet normally indicated for a wide variety of conditions in the Ayurvedic, Unani, and traditional Chinese systems of culling medicine.[40] [41] [42] [43] [44] [45] [46] Unani is based on a form of humorism, and and so in that system, bloodletting is used to correct supposed humoral imbalance.
Encounter likewise [edit]
- Alternative medicine
- Bloodstopping
- Blood donation
- Cupping therapy
- Hematology
- History of medicine
- Trepanation
- Humorism
- Fleams
- Barber's Pole
- Panacea
References [edit]
- ^ "Bloodletting". British Science Museum. 2009. Archived from the original on 15 April 2009. Retrieved 12 July 2009.
- ^ a b B.) Anderson, Julie, Emm Barnes, and Enna Shackleton. "The Art of Medicine: Over two,000 Years of Images and Imagination [Hardcover]." The Art of Medicine: Over 2, 000 Years of Images and Imagination: Julie Anderson, Emm Barnes, Emma Shackleton: ISBN 978-0226749365: The Ilex Press Limited, 2013.
- ^ Mestel, Rosie (half-dozen Baronial 2001). "Modern Bloodletting and Leeches". Los Angeles Times . Retrieved 12 July 2009.
- ^ "Why fair tests are needed". jameslindlibrary.org. 2009. Archived from the original on ii January 2007. Retrieved 8 January 2017.
- ^ Phlebotomy (book). Bonnie Yard. Davis. 2001. ISBN978-0-7668-2518-v . Retrieved 12 July 2009.
- ^ "The Ground of Therapeutic Phlebotomy". James C. Barton, Thousand.D. 2009. Retrieved 12 July 2009.
- ^ "Therapeutic Phlebotomy". Carteret General Hospital. 2009. Archived from the original on 7 July 2009. Retrieved 12 July 2009.
- ^ Williams, William F. (2013). Encyclopedia of Pseudoscience: From Alien Abductions to Zone Therapy. Routledge. ISBN978-1135955298.
- ^ Papavramidou, Niki; Thomaidis, Vassilios; Fiska, Aliki (December 2011). "The ancient surgical bloodletting method of arteriotomy". Journal of Vascular Surgery. 54 (half dozen): 1842–44. doi:10.1016/j.jvs.2011.05.100. PMID 21908152.
- ^ Parapia, Liakat Ali (September 2008). "History of bloodletting by phlebotomy". British Journal of Haematology. 143 (4): 490–95. doi:10.1111/j.1365-2141.2008.07361.ten. PMID 18783398. S2CID 9589933.
- ^ Schneeberg, NG (December 2002). "A twenty-first century perspective on the ancient art of bloodletting". Transactions & Studies of the College of Physicians of Philadelphia. 24: 157–85. PMID 12800324.
- ^ Stern, Heinrich (1915). Theory and Practise of Bloodletting. New York: Rebman Company. p. 9. Retrieved xx Baronial 2018.
- ^ Davis, Audrey; Appel, Toby (1979). Bloodletting Instruments in the National Museum of History and Technology . Washington, DC: Smithsonian Institution Press. p. 1. hdl:10088/2440.
- ^ Kean, Sam (2018). "Sweating blood". Distillations. iv (2): v. Retrieved 20 Baronial 2018.
- ^ Mikhail, Alan (2014). The Beast in Ottoman Arab republic of egypt. Oxford: Oxford University Printing. p. 169. ISBN978-0190655228 . Retrieved 20 August 2018.
- ^ "Degeneration of Medicine and the Grisly Art of Slicing Open Arms". BBC. 29 November 2002. Retrieved 12 July 2009.
- ^ Encyclopedia of ancient Greece. Nigel Guy Wilson. 2006. ISBN978-0-415-97334-2 . Retrieved 12 July 2009.
- ^ Coutinho, Elsimar Chiliad. (1999). Is Menstruation Obsolete?. Oxford University Press. ISBN0-19-513021-9.
- ^ Western medical thought from artifact to the Middle Ages. Mirko D. Grmek, Bernardino Fantini, Antony Shugaar. Cambridge, Ma.: Harvard University Press. 1998. ISBN0-674-40355-10. OCLC 39257545.
{{cite book}}: CS1 maint: others (link) - ^ The Western medical tradition : 800 B.C.–1800 A.D. Lawrence I. Conrad, Wellcome Found for the History of Medicine. Cambridge, Eng.: Cambridge Academy Press. 1995. ISBN0-521-38135-5. OCLC 31077045.
{{cite volume}}: CS1 maint: others (link) - ^ a b Conrad, Lawrence I. (1995). The Western Medical Tradition: 800 B.C.–1800 A.D. Cambridge, Eng.: Cambridge UP. ISBN0-521-38135-5.
- ^ Clutterbuck, Henry (1838). Dr Clutterbuck's Lectures On Bloodletting: Lecture 1. The London Medical Gazette.
- ^ Rangachari, P. K. (1997). "Evidence-based medicine: old French vino with a new Canadian label?". J R Soc Med. 90 (5): 280–84. doi:10.1177/014107689709000516. PMC1296268. PMID 9204029.
- ^ Carter (2005) p. vi
- ^ Lydia Kang MD & Nate Pederson, Quackery: A Brief History of the Worst Ways to Cure Everything "Drain Yourself to Bliss" (Workman Publishing Company; 2017)
- ^ Carter (2005) p. 7
- ^ During the Yellow Fever this do was as well used past Dr. Blitz. Read the book Fever 1793 for more info of look up Yellow Fever or Dr. Ben Rush Delpech, M (1825). "Example of a Wound of the Correct Carotid Artery". Lancet. 6 (73): 210–thirteen. doi:10.1016/S0140-6736(02)83521-8. quoted in Carter (2005):7–8
- ^ The Permanente Journal Volume 8 No. two: The asphyxiating and exsanguinating expiry of president george washington, p. 79, Spring, 2004, retrieved on 11 November 2012
- ^ a b Greenstone, Gerry (January–Feb 2010). "The history of bloodletting". British Columbia Medical Journal. 52 (1). Retrieved 17 February 2017.
- ^ Upshaw, John (2000). "The medicinal leech: Past and present". The American Surgeon. 66 (3): 313–14. PMID 10759207.
- ^ Warner, John Harley (July 1980). "Therapeutic explanation and the Edinburgh bloodletting controversy: 2 perspectives on the medical meaning of science in the mid-nineteenth century". Medical History. 24 (3): 241–58. doi:10.1017/s0025727300040308. PMC1082653. PMID 6997652.
- ^ a b Anders, Eli Osterweil (2016). "'A Plea for the Lancet': Bloodletting, Therapeutic Epistemology, and Professional Identity in Tardily Nineteenth-century American Medicine". Social History of Medicine. 29 (4): 781–801. doi:10.1093/shm/hkw026.
Arguing that it was the physician's obligation to be active and to arbitrate when necessary, bloodletting proponents explicitly assorted themselves with advocates of expectant treatment, whom they portrayed every bit passive, timid, and unwilling to do what was necessary to save their patients.
- ^ "Bloodletting". British Medical Journal. 1 (533): 283–91. 18 March 1871. doi:10.1136/bmj.1.533.283. PMC2260507.
- ^ "Bloodletting". UCLA Library: Biomedical Library History and Special Collections for the Sciences. 12 January 2012. Archived from the original on 13 March 2012. Retrieved v January 2012.
- ^ Ryan, Terence J (2015). "Osler and his didactics: relevant today". Postgraduate Medical Journal. 91 (1080): 540–41. doi:10.1136/postgradmedj-2015-133677. PMID 26404786. S2CID 41284621.
- ^ Tuttle, Kelly (2012). "Permit information technology bleed". Scientific discipline History Magazine. 30 (2): 17. Retrieved xx August 2018.
- ^ Merryweather-Clarke, Alison T.; Worwood, Mark; Parkinson, Lisa; Mattock, Chris; Pointon, Jennifer J.; Shearman, Jeremy D.; Robson, Kathryn J. H. (May 1998). "The effect of HFE mutations on serum ferritin and transferrin saturation in the Jersey population". British Journal of Haematology. 101 (2): 369–73. doi:ten.1046/j.1365-2141.1998.00736.ten. PMID 9609537. S2CID 19683918.
- ^ Powell, Lawrie West; Seckington, Rebecca C; Deugnier, Yves (2016). "Haemochromatosis". The Lancet. 388 (10045): 706–16. doi:x.1016/s0140-6736(15)01315-x. PMID 26975792. S2CID 208791894.
- ^ Cook, Lynda S. (2010). "Therapeutic Phlebotomy". Journal of Infusion Nursing. 33 (2): 81–88. doi:10.1097/nan.0b013e3181d00010. PMID 20228645.
- ^ Lone AH; Ahmad T; Anwar Yard; Habib Southward; Sofi G; Imam H (2011). "Leech therapy – a holistic approach of treatment in unani (greeko-arab) medicine". Anc Sci Life. 31 (1): 31–35. PMC3377041. PMID 22736888.
- ^ Unani System of Medicine Exercise, Globinmed.com.
- ^ Ayurveda – Panchakarma Archived xxx March 2013 at the Wayback Auto, holistic-online.com.
- ^ Ayurveda, Cancer.org.
- ^ Haemorrhage Peripheral Points: An Acupuncture Technique
- ^ Treating Herpes Zoster (Shingles) with Bloodletting Therapy: Acupuncture and Chinese Medicine Archived 2013-06-04 at the Wayback Machine
- ^ Chen PD, Chen GZ, Xu YX (2011). "Study strategies for bloodletting therapy in handling of acute soft tissue injuries". Zhong Xi Yi Jie He Xue Bao. 9 (3): 237–41. doi:x.3736/jcim20110302. PMID 21419074.
Books cited [edit]
- Carter, 1000. Codell; Barbara R. Carter (2005). Childbed fever. A scientific biography of Ignaz Semmelweis. Transaction Publishers. ISBN978-i-4128-0467-7.
- Carter, Thou. Codell (2012). The Refuse of Therapeutic Bloodletting and the Plummet of Traditional Medicine. New Brunswick & London: Transaction Publishers. ISBN 978-1-4128-4604-ii.
- Kang, Lydia; Nate Pederson (2017). Quackery: A Brief History of the Worst Ways to Cure Everything. Workman Publishing Company. [ ISBN missing ]
Farther reading [edit]
- McGrew, Roderick. Encyclopedia of Medical History (1985), cursory history pp. 32–34[ ISBN missing ]
External links [edit]
- The History and Progression of Bloodletting
- Medical Antiques: Scarification and Haemorrhage
- Pictures of antique bloodletting instruments
- PBS'due south Ruby Aureate: The Story of Blood
- Huge collection of antique bloodletting instruments
- "Breathing a Vein" phisick.com fourteen Nov 2011
Source: https://en.wikipedia.org/wiki/Bloodletting
0 Response to "Bloodlet in Out"
Post a Comment